With Brain Implants, Scientists Has Found A New Way To Treat Depression
Dhir Acharya - Dec 02, 2018
Scientists have found a new target for brain stimulation in depression treatment.
- IIT-Madras Aims To Interpret Brain Signals Into Language
- Sciencists Explains Why We Often Make Wrong Decisions
- Man Got A Car Key Implant In His Hand To Unlock His Tesla Just By Waving
In the past few years, doctors have found an unorthodox way to treat patients with depression, who did not respond to other methods: DBS, aka Deep Brain Stimulation. In particular, doctors will send accurate electrical shocks directly to certain areas of a patient’s brain. Though we cannot deny the positive effects, the method’s inconsistency poses concerns.
However, a new study at the University of California, San Francisco, appears to make an innovation in DBS therapy. According to the research, published in Current Biology on Thursday, there is another potential stimulation target that may bring about more consistent improvements in the patient’s mood. Moreover, with the new target, the patient doesn’t have to worry about side effects like mania in traditional BDS.
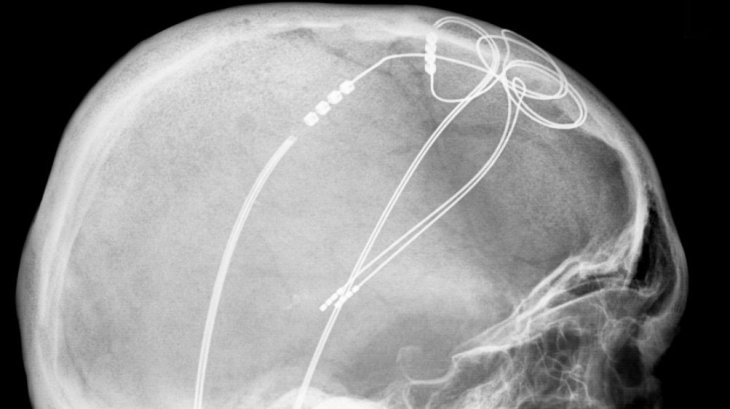
Usually, doctors use DBS to monitor neurological conditions such as epileptic seizures and Parkinson disease. Each condition is caused by erratic electrical activity in a specific area of the brain; in DBS, doctors implant electrodes in the patient’s brain through surgery and control them with a device implanted in the body, send impulses via these electrodes.
So, in DBS, the impulses, as pacemakers, restore a healthy brain pattern temporarily and reduce the patient’s symptoms. It is likely that depression patients’ brains work abnormally; hence, DBS can theoretically help difficult, treatment-resistant patients.
The researchers of the current study took the chance to do a unique experiment. Specifically, they experimented on 25 patients suffering from chronic epilepsy, who were planning to take an electrode implanting surgery.
The implants will record the activity of the neural network within a targeted brain area, from which doctors can then identify the source of the patient’s seizures. Next, they can make a plan to safely remove the brain parts that are affected later. But in this experiment, they could make use of the same implants to mimic a DBS session.
Doctors positioned the implants in different areas of the brain, including one close to the lateral portion of OFC (orbitofrontal cortex), which is right behind the eye. The OFC’s role is to make decisions, process emotions and regulate moods. And though OFC also contributes to depression, scientists haven’t considered it a target for stimulation.
For many days, doctors stimulated different regions on the volunteers’ brains through DBS, they did not exclude the OFC. Sometimes, doctors gave patients a sham stimulation instead, which operated as a control. Plus, after every session, patients talked to doctors about their feelings and answered questionnaires to assess their mood.
The patients had different initial depression symptoms levels, ranging from minimal to severe. There were no mood changes in the patient with little or no signs of depression, regardless of the stimulated regions and whether or not they were stimulated. However, the mood was boosted in patients that have moderate to severe level of depression symptoms. The changes came in just several minutes after their OFC were stimulated.
Furthermore, in comparison with the stimulation in other brain parts, the OFC stimulation seems to generate more reliable mood boosts, which means the larger the shocks, the greater the boosts.
Heather Dawes, the study author, a co-director of the Systems-Based Neurotechnology for Emerging Therapies program, UCSF, said that these findings are critical as they bring about a new possible target for mood symptoms treatment through brain stimulation therapies.
Plus, the implants allow researchers to record what the patients’ brains do outside of the sessions of DBS, meaning they can gain a better understanding of how DBS is affecting the OFC. Particularly, after the stimulation session, the patients’ brains appeared to resemble the level of activity observed when they were naturally feeling happy.
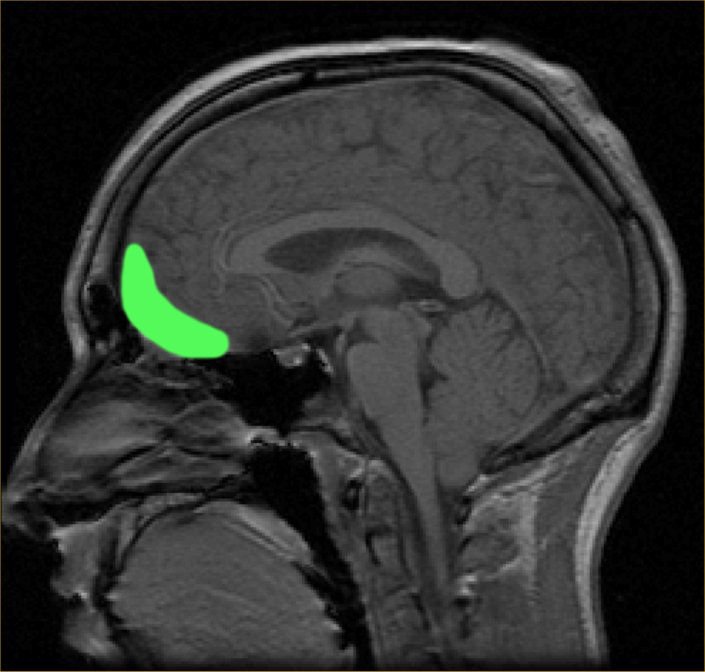
The orbitofrontal cortex (OFC)
According to Dawes, this shows that the stimulation is probably encouraging the brain to work on positive mood, rather than generating unnatural brain activity.
More importantly, patients did not experience any side effects.
Researchers have already established some targets for DBS depression therapy like the subgenual cingulate cortex, which is related to the regulation of moods and emotions. Nevertheless, DBS treatment did not prove to bring a consistent benefit.
Most importantly, a large DBS clinical trial in 2013 was stopped early because the situation of the patients did not improve as well as researchers predicted, some even got worse.
Technically, the trail failed but did not put an end to the whole concept of DBS therapy.
At the six month mark, the time to decide whether to take in more patients for the trial, a lot of patients did not respond to DBS treatment, but over a long time, there were significant improvements spotted.
The researchers prepared to conduct more clinical trials, but it is critical to know if there were a better way to refine the treatment.
As theorized by the team, since the OFC interacts with other areas of the brain which connect aspects of emotion and mood, it can provide a more reliable benefit when stimulated. Little evidence has been found on whether non-invasive stimulation forms relating to the OFC can help the depressed or not.
After all, there’s still a lot to do before we can make sure of anything.
Featured Stories

Features - Jan 29, 2026
Permanently Deleting Your Instagram Account: A Complete Step-by-Step Tutorial

Features - Jul 01, 2025
What Are The Fastest Passenger Vehicles Ever Created?

Features - Jun 25, 2025
Japan Hydrogen Breakthrough: Scientists Crack the Clean Energy Code with...

ICT News - Jun 25, 2025
AI Intimidation Tactics: CEOs Turn Flawed Technology Into Employee Fear Machine

Review - Jun 25, 2025
Windows 11 Problems: Is Microsoft's "Best" OS Actually Getting Worse?

Features - Jun 22, 2025
Telegram Founder Pavel Durov Plans to Split $14 Billion Fortune Among 106 Children

ICT News - Jun 22, 2025
Neuralink Telepathy Chip Enables Quadriplegic Rob Greiner to Control Games with...

Features - Jun 21, 2025
This Over $100 Bottle Has Nothing But Fresh Air Inside

Features - Jun 18, 2025
Best Mobile VPN Apps for Gaming 2025: Complete Guide

Features - Jun 18, 2025
A Math Formula Tells Us How Long Everything Will Live
Read more

ICT News- Feb 18, 2026
Google's Project Toscana: Elevating Pixel Face Unlock to Rival Apple's Face ID
As the smartphone landscape evolves, Google's push toward superior face unlock technology underscores its ambition to close the gap with Apple in user security and convenience.

Mobile- Feb 16, 2026
Xiaomi Launches Affordable Tracker to Compete with Apple's AirTag
For users tired of ecosystem lock-in or high prices, the Xiaomi Tag represents a compelling, no-frills option that delivers core functionality at a fraction of the cost.

Mobile- Feb 17, 2026
Anticipating the Samsung Galaxy S26 and S26+: Key Rumors and Specs
The Samsung Galaxy S26 series is on the horizon, sparking excitement among tech enthusiasts.
Comments
Sort by Newest | Popular